Blue Cross Enrollment for Employees Who Previously Waived CoverageBlue Cross will allow a medical, dental and vision group special enrollment period (SEP) for fully insured and small business funding groups choosing to participate. This SEP event is in light of the COVID-19 pandemic and is intended to allow employees on groups to enroll that are not currently serving a group established eligibility waiting period and had previously waived group coverage. Here are the details:
2 Comments
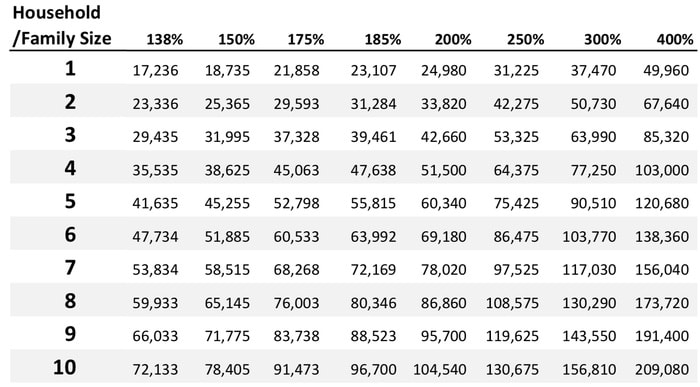
Just 11 days away! If you have not made your Open Enrollment appointment or finished your 2020 insurance enrollment with us, you are running out of time! To help us out, please send us your best estimate for your 2020 household income so we can get updated rates to you and help you with your 2020 plan selection. D O Y O U Q U A L I F Y F O R A. T A X C R E D I T ? Here are a few of the rules:
Learn more about Go365Insurance Commissioner Jim Donelon issued a cease and desist order today to United HealthCare Services, Inc. and/or UnitedHealthcare Insurance Company, its subsidiaries and affiliates (collectively hereafter referred to as “United”) for their intention to implement the removal of producer commissions from upcoming renewals of certain group health insurance products.
“In reviewing this situation I found it necessary to order the company to stop all efforts to implement such policy and to revise all applicable schedules of commissions and relevant rate and form filings to appropriately reflect the full commission payment required by law,” Commissioner Donelon stated. “This action is meant to both protect Louisiana’s health insurance producers who are due compensation and preserve our authority in making sure insurers writing in Louisiana are in compliance with our laws.” The Louisiana Department of Insurance (LDI) was contacted in May by numerous producers who indicated that they had been notified of United’s intention to implement a zero-dollar schedule of commissions applicable to all policies sold to groups of greater than 100 insureds with an effective date on or after September 1, 2019. Accompanying this notification was an inducement to work with United and affected insureds to negotiate a “replacement” agency fee to be paid by the insured to the producer and an offer by United to facilitate this payment. According to insurancenewsnet.com Health Agents for America President/CEO, Ronnell Nolan said, “It’s really appalling because our members have been fighting to get paid, and that bill is important. Lowering health care costs is what we want for our clients. But our members aren’t getting commissions on the individual market and UnitedHealthcare is not even paying for groups of 50 and above. So how can anybody point the arrow toward our members and say we’re part of the problem? We’re not part of the problem. Agents have been losing money since the passage of the ACA." |
Archives
June 2023
Categories
All
|






 RSS Feed
RSS Feed